Hospital Mergers: Are They Failing to Deliver on Cost Control Promises?
The debate surrounding hospital mergers continues to intensify, fueled by concerns that consolidation leads to higher prices and reduced access to care. Recent analysis challenges the widely held belief that these mergers create economic leverage, suggesting instead that hospitals struggling with market dominance are often financially unstable. This emerging data casts doubt on the efficacy of proposed solutions like hospital rate controls, prompting a reevaluation of healthcare market dynamics.
For years, a prevailing narrative has positioned hospital mergers as strategic maneuvers to gain market power and extract higher payments from insurers and patients. A recent paper, critiqued by healthcare futurist Jeff Goldsmith, posited that hospital mergers are conspiracies in restraint of trade, ultimately leading to advocacy for hospital rate controls as a corrective measure. However, new data from Trilliant Health paints a strikingly different picture.
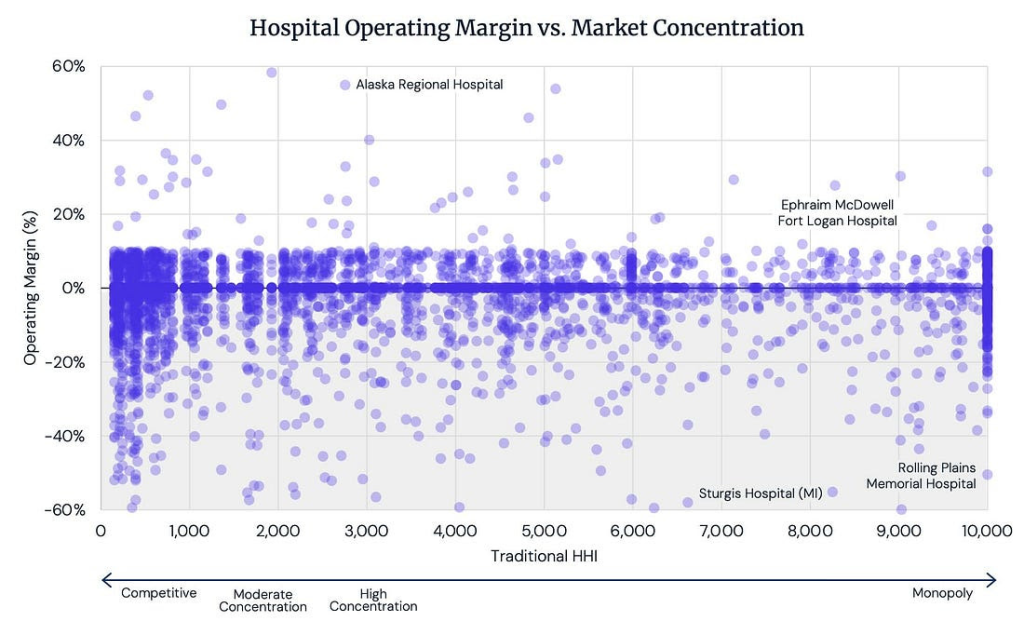
Source: Trilliant Healthcare Analysis of CMS HCRIS files (Hospital Cost Reports), 2023
The chart above, based on 2023 data, reveals a surprising lack of correlation between hospital operating margins and market concentration. In fact, hospitals with 100% local market share – those seemingly possessing the greatest monopolistic power – are often operating at a loss. According to Trilliant Health, the average hospital operating margin in 336 Core Based Statistical Areas (CBSAs) where hospital services are “controlled by a single firm” is -1.7%. This figure doesn’t even account for losses incurred by affiliated physician practices, suggesting the true financial strain on these dominant hospitals is even greater.
This data challenges the fundamental assumption that hospital mergers automatically translate into increased profitability. Instead, it suggests that hospitals may be struggling to manage costs and maintain financial viability, even in markets where they face limited competition. Could this indicate systemic issues within the healthcare system, such as inadequate reimbursement rates or inefficient operational practices?
The implications of these findings are significant. If hospital mergers aren’t driving up prices as feared, then the focus on rate controls may be misplaced. Perhaps a more effective approach would be to address the underlying factors contributing to hospital financial instability, such as rising labor costs, supply chain disruptions, and the increasing burden of uncompensated care. What other strategies could be employed to ensure the long-term financial health of hospitals and the accessibility of quality care for all?
The Complexities of Hospital Consolidation
Hospital consolidation has been a prominent trend in the healthcare industry for decades, driven by a variety of factors including economies of scale, increased bargaining power, and the desire to improve quality and efficiency. However, the impact of these mergers on healthcare costs and access remains a subject of intense debate.
Proponents of hospital mergers argue that consolidation can lead to cost savings through shared services, reduced administrative overhead, and increased negotiating leverage with suppliers. They also contend that larger hospital systems are better equipped to invest in advanced technologies and specialized services, ultimately improving the quality of care.
Critics, on the other hand, argue that hospital mergers often result in higher prices due to reduced competition. They point to studies showing that hospital prices tend to increase in markets where there are fewer hospital systems. Additionally, concerns have been raised about the potential for reduced access to care, particularly in rural areas where hospital closures following mergers can leave communities without local healthcare options.
The Federal Trade Commission (FTC) and the Department of Justice (DOJ) have been increasingly scrutinizing hospital mergers in recent years, seeking to prevent anti-competitive practices. However, successfully challenging a hospital merger can be difficult, as hospitals often argue that the benefits of consolidation outweigh the potential harms.
Understanding the nuances of hospital consolidation requires a careful consideration of the specific market conditions, the characteristics of the merging hospitals, and the potential impact on patients and communities. A one-size-fits-all approach is unlikely to be effective, and policymakers must tailor their responses to the unique challenges facing each healthcare market.
For further information on hospital consolidation and its impact, consider exploring resources from the Kaiser Family Foundation and the American Hospital Association.
Frequently Asked Questions About Hospital Mergers
-
What is the primary concern regarding hospital mergers?
The main concern is that hospital mergers reduce competition, potentially leading to higher prices for patients and insurers.
-
Do hospital mergers always result in increased profitability?
No, recent data suggests that hospitals with dominant market share are often operating at a loss, challenging the assumption that mergers automatically lead to higher profits.
-
What are hospital rate controls?
Hospital rate controls are government regulations that limit the amount hospitals can charge for their services.
-
What role do regulatory agencies play in hospital mergers?
The Federal Trade Commission (FTC) and the Department of Justice (DOJ) review hospital mergers to ensure they don’t violate antitrust laws.
-
What factors contribute to hospital financial instability?
Rising labor costs, supply chain disruptions, and the increasing burden of uncompensated care are all contributing factors.
-
Are there benefits to hospital consolidation?
Proponents argue that consolidation can lead to cost savings through shared services and increased investment in technology.
The evolving landscape of hospital finances demands a nuanced understanding of market dynamics. As we continue to grapple with the challenges of healthcare affordability and access, it’s crucial to move beyond simplistic narratives and embrace data-driven insights. Share this article with your network to spark a conversation about the future of healthcare.
Discover more from Archyworldys
Subscribe to get the latest posts sent to your email.

